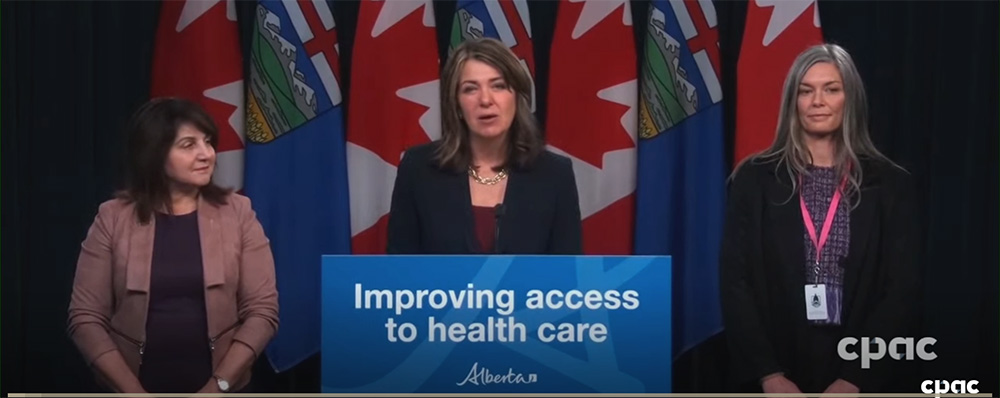
At Premier Danielle Smith and Health Minister Adriana LaGrange’s recent press conference, they announced new programs to “support nurse practitioners to work independently” to give Albertans better healthcare access.
“This new program removes barriers and empowers nurse practitioners to open their own clinics, take on patients, and offer services that reflect their full extent of training, skills, and experience,” said Premier Smith.
Smith added, “We know that too many Albertans do not have access to a primary-care practitioner, and often when they can find a healthcare provider, they still need to wait weeks to get an appointment. That’s just unacceptable.”
Ironically, however, that same day, Alberta Health gave Cochrane nurse practitioner Karen Parker some…we’ll say less than supportive news.
Parker has been working to open a first-of-its-kind nurse practitioner clinic in Cochrane for the last four years.
“This will be a catalyst for change across Canada,” Parker formerly said about her clinic.
It sounds like the kind of program Premier Smith claims her government is trying to bring to fruition.
A Nurse-Driven Solution
Parker’s proposed clinic was met with a mix of support and questions from Cochrane residents.


Her clinic model stirred hope and curiosity about what kinds of services it could and couldn’t provide.
Ultimately, with investors on board, deposits paid, and employees ready to go, the clinic was expected to open this summer.
The clinic was supposed to reduce the number of Cochranites without access to a family doctor by half, giving almost 20,000 people access to reliable healthcare.
The nurse-led clinic would have provided much-needed relief for an overburdened town health system, and it would have taken only ten nurse practitioners to do it.
“We’ve been advertising; we were organizing to start as soon as an equitable funding model was provided,” Parker told The Cochrane Eagle.
Instead of being paid fee-for-service, Parker’s nurse practitioners would be paid salaries, which aligns with the government’s previous primary care network model.
Equitable or Not?
However, Parker says Smith’s new health care plan is far from “equitable.”
She says what Alberta Health was willing to provide in salaries wasn’t feasible, forcing her to cancel the clinic’s planned opening.


“It’s non-viable – we would be losing money,” she said. “We’re excluded from even applying for this. It’s misleading, and it missed the mark significantly.”
Parker called this a “fundamental disconnect” between the government’s claims and the reality of what she would need to provide these services to the public.
Alberta Medical Association president Paul Parks reviewed Smith’s new health plan. Park said it could be “very positive,” depending on how much collaboration between nurse practitioners and family physicians is involved.
However, like Parker, he noted that the payment model seemed likely to cause practitioners to “have a hard time staying afloat.”
Under the government’s new funding model, nurse practitioner clinics will receive about 20 percent less funding than regular clinics – most of which already need help to stay open.
Where Should The Government Put Its Money?
Some doctors are skeptical about whether nurse practitioner clinics will fill the gap in primary healthcare.
High River physician Scott Repaske told the Edmonton Journal, “I don’t really think that [proposed model] is a good use of funds. You could give me a 25 percent raise in my fee codes, and it still probably wouldn’t cost as much. And you would immediately see a return of family docs back to the clinics.”
According to the United Nurses of Alberta, nurse practitioners can provide about eight out of ten of the services doctors provide. If more is necessary, patients would be referred to specialists as needed.
Parker’s clinic was going to employ ten nurse practitioners, each helping 1,000 patients, which would have reduced the number of Cochrane residents without a family doctor.
But alas, the funding levels proposed are not enough to make the clinic viable.
Regardless of lower-than-expected funding levels, the new system is still full steam ahead.
Over the next three years, the Nurse Practitioner Association of Alberta will receive a $2 million grant to help nurse practitioners through the new program application process and recruit and support new nurse practitioners in setting up their clinics.
That was the plan, but Parker’s experience raises the possibility that other nurses will go through the application and recruitment process just to learn that the funding for nurse practitioner clinics is insufficient to make their clinics viable.
The people of Cochrane are now left without medical options that could have been up and running this summer.






